The surgeons at Tampa Eye Clinic have helped thousands of people enjoy better vision. Leading the way with new medications and surgical procedures, Tampa Eye Clinic can diagnose and treat a wide range of diseases and conditions. We’re committed to providing our patients the most advanced care available.

To find out more about any of these conditions and their treatments, click on their links.
The human eye gives us the sense of sight, allowing us to learn more about the surrounding world than any of the other five senses. The eye allows us to see and interpret the shapes, colors and dimensions of objects by processing the light they reflect or give off.
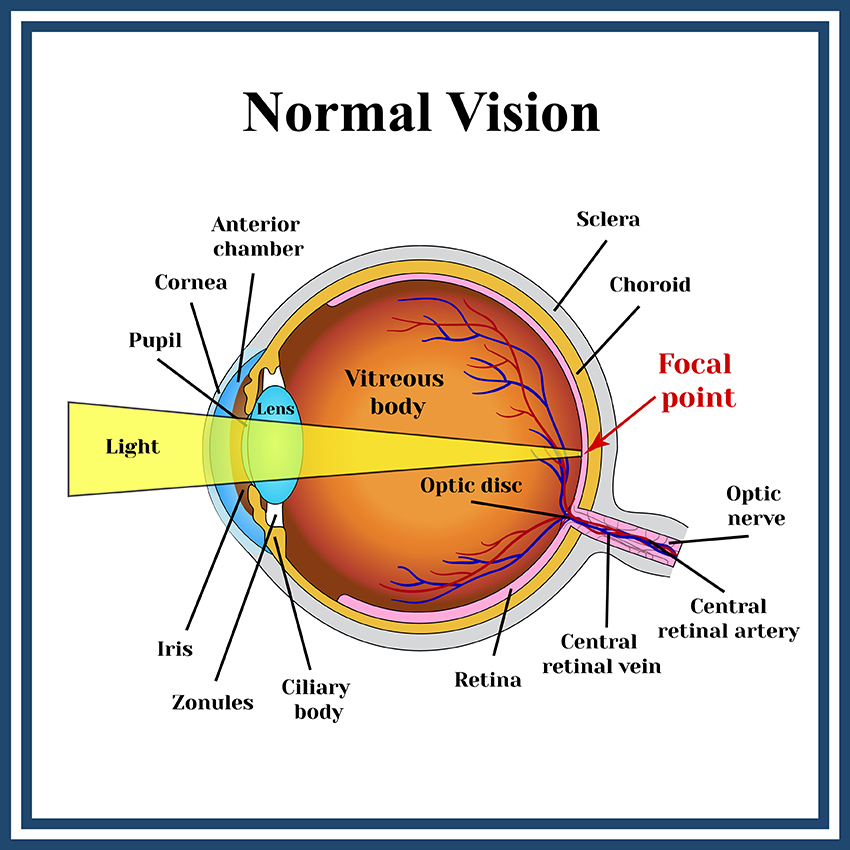
The cornea (the clear window on the front of the eye) and the lens of the eye (the transparent structure inside the eye) are both critical to normal vision. The goal of these two lenses is to focus light onto a layer on the back of the eye known as the retina. As light enters into the eye it is focused by the cornea and the lens so that images appear clearly on the retina. The retina then transmits these images to the brain where they are processed. If the images focus perfectly on the retina, this results in 20/20 vision; focusing in front or behind the retina results in nearsightedness or farsightedness. If the cornea is shaped like a football instead of a sphere, this is called astigmatism. When any of these conditions occurs, images are perceived by the brain as being blurry. This is due to “refractive error” which means the eyeball is not the right size or the cornea does not have the right curve.
Myopia, unlike normal vision, occurs when the cornea is too curved or the eye is too long. This causes light to focus in front of the retina, resulting in blurry distance vision.
Myopia is a very common condition that affects nearly 30 percent of the U.S. population. It normally starts to appear between the ages of eight and 12 years old, and almost always before the age of 20. As the body grows, the condition often worsens. It typically stabilizes in adulthood.

Many times, myopia is diagnosed during school screenings. Sometimes parents notice that their children are having difficulty seeing street signs or the television. Your eye doctor can conduct a refractive evaluation to determine whether your eyes focus light rays exactly on the retina at distance and near. A visual acuity test will determine your ability to see sharply and clearly at all distances. Your eye doctor will also check your eye coordination and muscle control, as well as your eyes’ ability to change focus. All of these are important factors in how your eyes see.
Glasses and contact lenses are used by many for the temporary treatment of myopia. However, there are a number of vision correction procedures that can surgically reduce or eliminate myopia.
Other types of refractive errors include: nearsightedness, farsightednes and presbyopia.
Hyperopia, unlike normal vision, occurs when the cornea is too flat in relation to the length of the eye. This causes light to focus at a point beyond the retina, resulting in blurry close vision and occasionally blurry distance vision as well. Usually this condition is undetected until later in life because the young eye is able to compensate for the hyperopia by contracting the internal lens of the eye.

Many people are not diagnosed with hyperopia without a complete eye exam. School screenings typically do not detect this condition because they test only for distance vision. Your eye doctor can conduct a refractive evaluation to determine whether your eyes focus light rays exactly on the retina at distance and near. A visual acuity test will determine your ability to see sharply and clearly at all distances. Your eye doctor will also check your eye coordination and muscle control, as well as your eyes’ ability to change focus. All of these are important factors in how your eyes see.
Glasses and contact lenses are used by many for the temporary treatment of hyperopia. However, there are a number of vision correction procedures that can surgically reduce or eliminate hyperopia.
Other types of refractive errors include: nearsightedness and presbyopia.
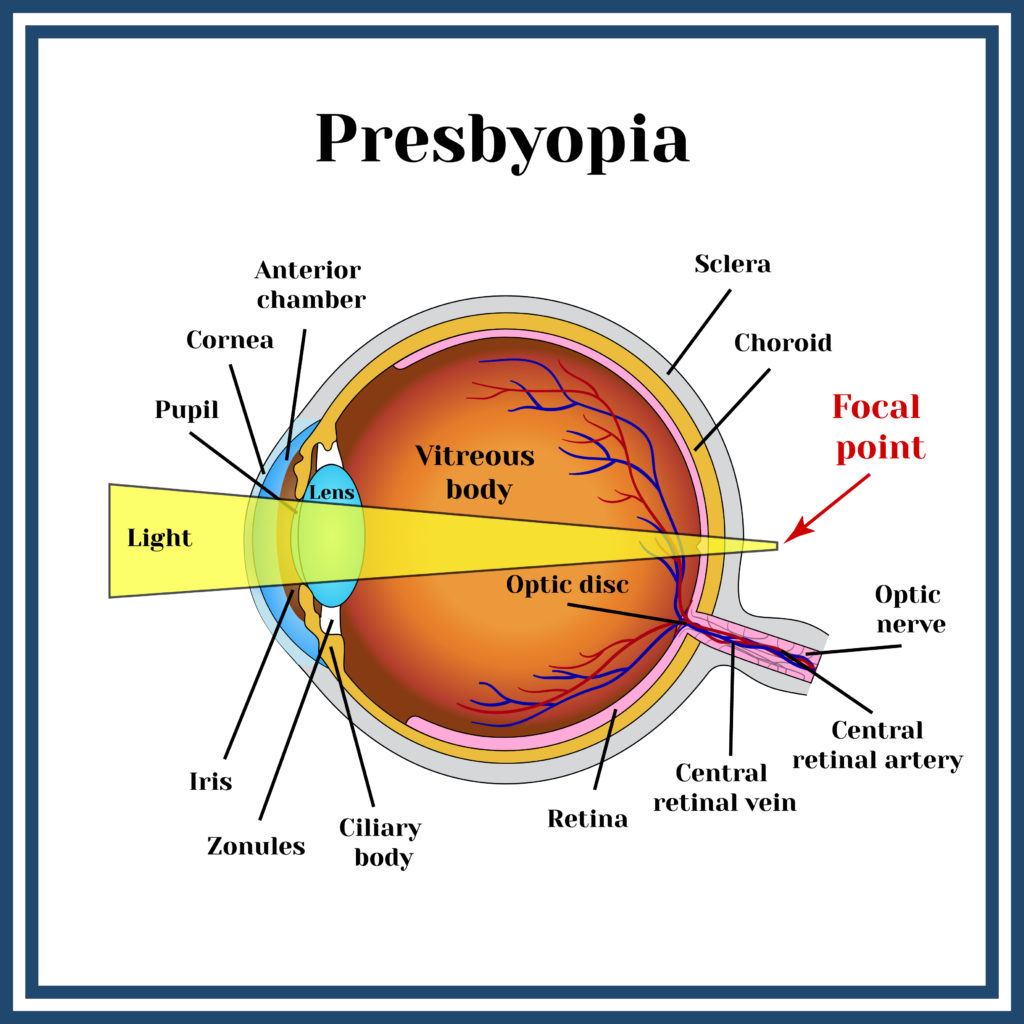
Presbyopia is a vision condition in which the lens loses its flexibility, making it difficult to focus on close objects. During the early and middle years of life, the crystalline lens of the eye has the ability to focus both near and distant images by getting thicker for near objects and thinner for distant objects. When this ability is lost, presbyopia results. Presbyopia usually becomes noticeable in the early to mid-forties.
A comprehensive examination will include testing for presbyopia. Your eye doctor can conduct a refractive evaluation to determine whether your eyes focus light rays exactly on the retina at distance and near. A visual acuity test will determine your ability to see sharply and clearly at all distances. Your eye doctor will also check your eye coordination and muscle control, as well as your eyes’ ability to change focus. All of these are important factors in how your eyes see.
Reading glasses and contact lenses are used by many for the temporary treatment of presbyopia. However, there are a number of vision correction procedures that can surgically reduce or eliminate the effects of presbyopia. Some presbyopic patients like monovision, which allows them to see distance clearly in one eye and close-up clearly with the other eye.
Presbyopia can be present in combination with other types of refractive errors such as nearsightedness, farsightednes and astigmatism.
Monovision is a technique used to correct presbyopia. In monovision, one eye is corrected for distance vision while the other eye is corrected for near vision. This approach can be achieved through contact lenses, refractive surgery, or intraocular lenses.
Here’s how it works:
The brain learns to favor one eye over the other depending on the visual task, allowing the person to see both near and far without the need for bifocals or reading glasses. Most people’s brains automatically get used to monovision within a couple of weeks or months. However, some people may find it challenging to adapt to monovision, as it can affect depth perception and may cause visual discomfort or difficulty in low-light conditions.
If you are considering a vision correction procedure, your doctor can put you into monovision contact lenses so you can try it before you permanently correct your eyes with monovision.
In our experience, most people over the age of 40 to 45 who try monovision and take the time to fully become accustomed to it, like it and find it very useful.
As we age, the lenses in the eyes lose some of their elasticity, and without elasticity they lose some of their ability to change focus for different distances.
Presbyopia may seem to occur suddenly, but the actual loss of flexibility takes place over a number of years.
Long before an individual is aware that seeing close up is becoming more difficult, the lenses in the eyes have begun losing their ability to flatten and thicken. Only when the loss of elasticity impairs vision to a noticeable degree is the change recognized.
Astigmatism is a common vision condition resulting from an irregular curvature of the cornea or lens in the eye. This irregular shape prevents light from focusing properly on the retina, leading to blurred or distorted vision at any distance. It often occurs alongside other refractive errors like myopia (nearsightedness) or hyperopia (farsightedness).

Diagnosis is typically made through a comprehensive eye examination.
Premium IOL Options:
Crystalens Advances in Intraocular Lens (IOL) technology now provide a reliable and effective option for patients with astigmatism. Until the recent introduction of Toric IOLs, people who were considered candidates for intraocular lenses could only have their nearsightedness and farsightedness corrected during lens implant surgery. Patients with astigmatism had to either have corneal refractive surgery (LASIK, PRK, or Limbal Relaxation Incisions) after lens implant surgery or remain dependent on glasses or contacts.
Toric IOLs are specially shaped IOLs designed to offset the imbalance created by the irregular shape of the cornea. Once implanted and aligned inside the eye, they stay fixed in place thereby eliminating pre-existing astigmatism.
There are several manufacturers of Toric IOLs that are available to correct various amounts of astigmatism. Your doctor will select the Toric IOL that is best suited for your eye condition. Toric IOLs are considered “premium” IOLs which means there will be additional costs associated with these lenses.
The cornea is the clear front window of the eye. It transmits light to the interior of the eye allowing us to see clearly. Corneal disease is a serious condition that can cause clouding, distortion and eventually blindness. There are many types of corneal disease. The three major types are keratoconus, Fuchs’ endothelial dystrophy and bullous keratopathy.

Keratoconus is a weakening and thinning of the central cornea. The cornea develops a cone-shaped deformity. Progression can be rapid, gradual or intermittent. Keratoconus usually occurs in both eyes, but can occur in only one eye.
Fuchs’ endothelial dystrophy is a hereditary abnormality of the inner cell layer of the cornea called the endothelium. The purpose of this layer is to pump fluids out of the cornea, keeping it thin and crystal clear. When the endothelium is not healthy, fluids are not pumped out and the cornea develops swelling, causing it to become cloudy and decrease vision.
Bullous keratopathy is a condition in which the cornea becomes permanently swollen. This occurs because the inner layer of the cornea, the endothelium, has been damaged and is no longer pumping fluids out of the tissue.
Your eye doctor can check for corneal disease and trauma by examining your eyes with magnifying instruments. Using a slit lamp and advanced diagnostic technologysuch as corneal topography, your doctor can detect early cataracts, corneal scars, and other problems associated with the front structures of the eye. After dilating your eyes, your doctor will also examine your retina for early signs of disease.
As with any serious eye infection, corneal disease should be treated immediately. Although corneal transplant is almost always the necessary treatment to restore vision when the cornea becomes clouded, there are other measures that can be taken to prolong vision in the early stages of disease.
Fuchs’ dystrophy (named after Dr. Fuchs) is an inherited condition that affects the delicate inner layer (endothelium) of the cornea. Patients with Fuchs’ dystrophy have endothelial cells that:

Although doctors can often see early signs of Fuchs’ dystrophy in people in their 30s and 40s, the dystrophy rarely affects vision until people reach their 50s and 60s.
The cornea is the clear “window” in the front of the eye that allows light rays to enter.
The cornea has three layers – the outer epithelium (or skin), a middle area called stroma and a delicate, single celled inner lining called the endothelium. The endotheliumacts as a barrier to prevent water inside the eyeball from moving into and swelling the other layers of the cornea. The cells of the endothelium actively pump water from the cornea back into the eye.
If the endothelium does not function normally, then water moves into the cornea causing swelling. Swelling causes clouding of the cornea and blurred vision. The more corneal swelling or “edema,” the more severely the vision is blurred. Eventually, the outer corneal layer (epithelium) also takes on water, resulting in pain and more severe vision impairment. Epithelial swelling reduces vision by changing the normal curvature of the cornea. It causes a sight-limiting haze to develop. Epithelial swelling may also form small “blisters” on the corneal surface. When these “blisters” burst, extreme pain can occur.
In early stages, people with Fuchs’ dystrophymay wake upwith blurred vision, which gradually clears over the day. That’s because during the day, water continuously evaporates from the surface of the eye and is replaced with water drawn from the inner compartments of the eye. Overnight, when we sleep with closed eyes, water cannot evaporate from the surface of the eye and accumulates in the cornea, causing slight swelling which blurs vision. Once eyes are opened throughout the day, evaporation reduces the water content and the thickness of the cornea, allowing for clearing of vision. In later stages, as the dystrophy worsens, evaporation is not enough to remove accumulated water in the cornea, and swelling and blurred vision last all day.
Endothelial cells can be counted with special photographic methods. Most people are born with approximately 4,000 cells per square millimeter of the endothelial surface. These cells do not divide and cannot reproduce or replace themselves. As we age, we gradually lose endothelial cells.
|
Age
|
Endothelial Cell Density
|
|---|---|
|
Infant
|
3,000 – 4,000 / sq. mm
|
|
Teenager
|
3,000 / sq. mm
|
|
Adult
|
2,500 – 3,000 / sq. mm
|
|
Elderly
|
2,000 – 2,500 / sq. mm
|
Fuchs’ dystrophy is detected by examining the cornea with a slit lamp microscope that magnifies the endothelial cells thousands of times. The health of the endothelium is evaluated and monitored with pachymetry (which measures the thickness of the cornea) and specular microscopy (which photographs the cells for counting). As the dystrophy becomes more advanced, corneal clouding may make counting the cells impossible.
Fuchs’ dystrophy cannot be cured. Doctors are unable to treat the endothelial cells to make them work better or to become more numerous. However, blurred vision resulting from the corneal swelling can be controlled with medication. Salt solutions containing sodium chloride (Muro 128 drops or ointment, 2% or 5%) are often prescribed to draw fluid from the cornea and reduce swelling. Steroid eye drops may be helpful in specific situations.
Another simple technique that reduces moisture in the cornea is to hold a hair dryer at arm’s length, blowing air towards the face with the eyes open. This warm air flow increases evaporation of water from the cornea, temporarily decreases swelling, and may improve vision. Often very helpful in early stages, this technique may not be effective when swelling is severe, as in advanced stages.
Corneal transplantationis considered when vision deteriorates to the point that it interferes with daily activities and impairs a person’s ability to function normally. This surgery replaces the full thickness of the cornea, including the endothelium, with healthy layers. The cloudy cornea is replaced with clear corneal tissue.
The cornea is the clear, outer window of the eye. A corneal abrasion is simply a scratch in the epithelium (skin), or the thin, outer layer of the cornea. Abrasions usually heal in a short time period, sometimes within hours. Deeper or larger scratches may take up to a week. The cornea has a tremendous number of nerve endings, which makes any damage to the cornea very painful.

Your eye doctor can identify corneal abrasions by examining your eyes with magnifying instruments. Your doctor will check your eye, including under your eyelid, to make sure there are no foreign materials present. Depending on the initial exam, fluorescein dye may be used to help locate and identify the corneal abrasions. A test called the Seidel test (painting the wound with dye and observing for leakage) may be performed to uncover possible deeper injuries.
Your doctor may apply a topical anesthesia to help relieve the pain. Usually, a tight patch will be placed over the eye and if the abrasion is small, the epithelium should heal overnight. If the abrasion is large, it may take a few days and your doctor may prescribe antibiotics to help prevent infections. It is important that you do not rub your eye, especially during the healing process.
The front portion of the eye is covered with a thin, transparent membrane called the cornea, which protects the interior of the eye. If there is a break or defect in the surface layer of the cornea, called the epithelium, and damage to the underlying stroma, a corneal ulcer results. The ulcer is usually caused by microrganisms, which gain access to the stroma through the break in the epithelium.

Corneal ulcers generally heal well if treated early and aggressively. However if neglected, corneal clouding and even perforation (a hole in the cornea) may develop, resulting in serious loss of vision and possibly loss of the eye. Corneal ulcers are a serious vision-threatening condition and require prompt medical attention.
Your eye doctor can identify corneal ulcers by examining your eyes with magnifying instruments and performing a culture study to identify infection. Your doctor will check your eye, including under your eyelid, to make sure there are no foreign materials present. Depending on the initial exam, fluorescein dye may be used to identify the corneal defects. A test called the Seidel test (painting the wound with dye and observing for leakage) may be performed to uncover possible deeper injuries.
If treated early, corneal ulcers are usually curable in two to three weeks. They are typically treated with antibiotic eye drops. Sometimes, topical steroids will also be used to decrease the risk of scarring and inflammation.
The name “dry eye” can be a little confusing since one of the most common symptoms is excessive watering! It makes more sense, though, when you learn that the eye makes two different types of tears.

Tears produced slowly and steadily throughout the day. Lubricating tears contain a precise balance of mucous, water, oil, nutrient proteins, and antibodies that nourish and protect the front surface of the eye. If your eye is not producing enough lubricating tears, you have dry eye.
These tears do not have much lubricating value. Reflex tears serve as a kind of emergency response to flood the eye when it is suddenly irritated or injured. Reflex tears might occur when you get something in your eye, when you’re cutting onions, when you’re around smoke, or when you accidentally scratch your eye. The reflex tears gush out in such large quantities that the tear drainage system can’t handle them all and they spill out onto your cheek. Still another cause of reflex tearing is irritation of the eye from lack of lubricating tears.
Your eye doctor can check for dry eye by examining your eyes with magnifying instruments, measuring your rate of tear production and checking the amount of time it takes for tears to evaporate between blinks. The doctor can also check for pinpoint scratches on the front surface of the eye caused by dryness using special, colored eyedrops call fluorescein or Rose Bengal.
The most common treatment is use of artificial teardrops that help make up for the lack of natural lubricating tears. Artificial tear products come in liquid form, longer lasting gelform and long-lasting ointment form, which is most often recommended for nighttime use. Many different brands of artificial tears are available over-the-counter. Some contain preservatives and some do not. Unpreserved tears may be recommended for people whose eyes are sensitive to preservatives. Artificial tears can generally be used as often as needed, from a few times per day to every few minutes. You should follow the regimen your doctor recommends.
When infection, inflammation of the eyelids or clogged oil glands contribute to dry eye, special lid cleaning techniques or antibiotics may be recommended. It may also help to avoid hot, dry or windy environments or to humidify the air in your home or office.
Restasis is an exciting new treatment for Dry Eye Disease. Restasis drops help the eyes produce more tears by reducing inflammation, which is often a cause of dry eye. Unlike artificial tears, Restasis is the first drug proven to effectively treat a cause of Dry Eye Disease rather than only temporarily alleviate symptoms.
Punctal occlusion is a medical treatment for dry eye that may enable your eyes to make better and longer use of the few lubricating tears they do produce.
We now have the ability to provide our patients with a more natural substitute for the tears that they’ve lost. It’s called Platelet Rich Plasma (PRP) tears. PRP tears are derived from a person’s own body. This is accomplished by taking platelets and plasma from the patient’s blood and mixing them with saline to create personalized, nutrient rich, growth factor rich natural tears. This protocol has been shown to help people with Dry Eyes, Recurrent Corneal Erosions, certain Corneal Dystrophies (Map, Dot, Fingerprint), and non-healing Corneal Ulcers. It’s a step into the world of Regenerative Medicine. A second option that we now offer involves using Broad Based Light (BBL) to help patients who have Rosacea that causes dry eyes. People with facial redness or redness on the eyelids often have problems generating the natural oil component of the natural tear solution. This oil is important because it prevents the liquid part of the tears from evaporating too quickly.
These treatments are not currently covered by insurance. Please contact our office for more information. These two new treatment approaches have created a marked improvement in patients’ suffering from Dry Eye. We are happy to be of service to patients suffering from this condition.
Blepharitis means inflammation of the eyelids. Some doctors call it granulated eyelids. Almost everyone gets blepharitis at some time in his or her life. Some people get it repeatedly. Fortunately, blepharitis is relatively easy to treat.

If you think you may have blepharitis, your eye doctor can determine the cause and recommend the right combination of treatment specifically for you. You doctor will perform a complete eye examination to determine the most effective treatment.
In addition to eliminating redness and soreness, treatment can prevent potential infection and scarring of the cornea.
Cleaning
Usually, blepharitis can be controlled by careful, daily cleaning of the eyelashes. You can do this by moistening a clean washcloth with tap water as warm as you can stand without burning. Hold the washcloth against the eyelids until it cools, then rewarm and repeat for five to ten minutes.
After soaking, scrub each eyelid gently for one minute using a clean washcloth wrapped around your index finger and moistened with warm tap water. Cotton-tipped applicators, like Q-tips, are also useful to remove accumulated material from the eyelashes.
To remove excessive amounts of material from your eyelids, use a few drops of a non-irritating shampoo, such as baby shampoo, mixed in lukewarm water. Being careful to avoid getting shampoo in your eye, scrub back and forth along the eyelashes of all eyelids, and then rinse with plain tap water. Once the redness and soreness are under control, this cleaning may be decreased from daily to twice weekly. However, if the symptoms return, return to daily cleansing immediately.
Medication
In some cases, your doctor may prescribe eye drops or ointment to be used along with the daily cleansing regimen. For ointments, use a clean fingertip to rub a small amount into the eyelashes. Be careful to follow recommended dosages; excess medication will cause temporary blurring of vision. And with any medication, there is a small possibility of allergy or other reaction. If you think this is happening, stop the medication and contact your doctor immediately.
For certain types of blepharitis, medications taken by mouth are helpful. Most of these medications are antibiotics that also improve or alter the oil composition of the eyelid oil glands. When taken properly, they are safe. However, side effects may occur in some individuals, including skin rash, slight nausea and increased sensitivity to sun.
Although medications may help control the symptoms of blepharitis, they alone are not sufficient; keeping the eyelids clean is essential.
Conjunctivitis (pink eye) is an inflammation of the conjunctiva, the thin, transparent membrane covering the surface of the inner eyelid and the front of the eye. The conjunctiva has many small blood vessels. It lubricates and protects the eye while the eye moves in its socket. When the conjunctiva becomes inflamed, this is called conjunctivitis.

If you think you may have blepharitis, your eye doctor can determine the cause and recommend the right combination of treatment specifically for you. You doctor will perform a complete eye examination to determine the most effective treatment.
In addition to eliminating redness and soreness, treatment can prevent potential infection and scarring of the cornea.
Cleaning
Usually, blepharitis can be controlled by careful, daily cleaning of the eyelashes. You can do this by moistening a clean washcloth with tap water as warm as you can stand without burning. Hold the washcloth against the eyelids until it cools, then rewarm and repeat for five to ten minutes.
After soaking, scrub each eyelid gently for one minute using a clean washcloth wrapped around your index finger and moistened with warm tap water. Cotton-tipped applicators, like Q-tips, are also useful to remove accumulated material from the eyelashes.
To remove excessive amounts of material from your eyelids, use a few drops of a non-irritating shampoo, such as baby shampoo, mixed in lukewarm water. Being careful to avoid getting shampoo in your eye, scrub back and forth along the eyelashes of all eyelids, and then rinse with plain tap water. Once the redness and soreness are under control, this cleaning may be decreased from daily to twice weekly. However, if the symptoms return, return to daily cleansing immediately.
Medication
In some cases, your doctor may prescribe eye drops or ointment to be used along with the daily cleansing regimen. For ointments, use a clean fingertip to rub a small amount into the eyelashes. Be careful to follow recommended dosages; excess medication will cause temporary blurring of vision. And with any medication, there is a small possibility of allergy or other reaction. If you think this is happening, stop the medication and contact your doctor immediately.
For certain types of blepharitis, medications taken by mouth are helpful. Most of these medications are antibiotics that also improve or alter the oil composition of the eyelid oil glands. When taken properly, they are safe. However, side effects may occur in some individuals, including skin rash, slight nausea and increased sensitivity to sun.
Although medications may help control the symptoms of blepharitis, they alone are not sufficient; keeping the eyelids clean is essential.